To help address inequities faced by patients treated for otolaryngologic and communication disorders at Duke, we implemented a Health Equity Curriculum for our faculty, staff, and trainees.
Patients who need our services may face unique challenges that aren’t broadly shared among other medical subspecialties, such as disparities in vaccination rates for certain racial and ethnic groups to prevent HPV-related head and neck cancers, as well as inequitable access to cochlear implantation in rural areas.
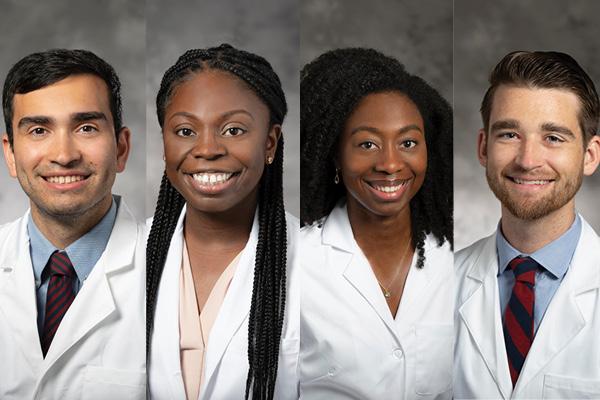
Led by residents Dr. Nicholas Frisco (PGY-3), Dr. Robbie Patterson (PGY-5), Dr. Somtochi Okafor (PGY-5), and Dr. Eseosa Odigie (PGY-2) — under the guidance of Dr. Trinitia Cannon — the curriculum seeks to equip departmental members with the knowledge and skills to address health disparities, promote research on health equity topics, and improve care and patient outcomes for marginalized populations.
“A health equity curriculum in residency training is crucial for preparing future physicians to provide comprehensive, culturally competent care,” Dr. Cannon said. “By understanding the social determinants of health, residents can better address disparities in healthcare access, quality, and outcomes. This training empowers doctors to advocate for vulnerable populations, implement equitable treatment strategies, and contribute to a more just healthcare system. Ultimately, a focus on health equity enhances the quality of care for all patients, regardless of their background or socioeconomic status.”
As part of our effort to address these issues, we hold recurring departmental grand rounds sessions focused on health equity topics, offer mentored quality improvement and research activities and support efforts to advance knowledge in the populations that we serve.
These efforts are having an increasing impact on our teams and department culture.
“The curriculum has helped me more frequently consider contextual factors in my patient encounters,” said Dr. Frisco. “For example, for things as simple as post-discharge diet recommendations, I consider how difficult it can be for some patients to have access to a soft, calorie-rich diet, and the need to lean on case workers/patient advocates to ensure that adequate resources are provided.”
Grand Rounds Increase Awareness
At ground rounds, invited experts share their research and work on health equity, put in the context of otolaryngology. They relay the experiences of their patients and the ways that our health system is currently failing to address key aspects of what they need.
Some highlights of those grand rounds include:
- Duke orthopaedic surgeon Erica Taylor, MD, MBA, spoke about the process of integrating health equity into one's academic practice at Duke and the barriers to implementation.
- Michelle Morris, MD, MPH, from the New York Department of Public Health, presented research on the impact of race on access to care.
- Regan Bergmark, MD, from Harvard’s Department of Otolaryngology Head and Neck Surgery, presented her research on some of the disparities that are faced within our field.
“I think that the grand rounds have increased the discussion and awareness of health inequities that our patients face at Duke,” said Dr. Patterson. “It’s provided a new perspective for people and understanding of the challenges that patients may face in accessing care.”
Mentoring Spurs Health Equity Research
In addition to expert lectures, residents can focus on health equity/health disparities questions during their dedicated research block with the help of dedicated curriculum mentors.
The curriculum currently has six mentors, both within and outside of the department, who help facilitate research projects addressing health inequity in conjunction with clinical/research faculty mentors from the department.
The mentors include:
Jamila Minga, PhD
Assistant Professor of Head and Neck Surgery & Communication Sciences
Assistant Professor in Neurology Member of the Center for Cognitive Neuroscience
Dennis Frank-Ito, PhD
Associate Professor in Head and Neck Surgery & Communication Sciences
Nosayaba Osazuwa-Peters, PhD, MPH, BDS
Associate Professor in Head and Neck Surgery & Communication Sciences
Associate Professor in Population Health Sciences
Assistant Research Professor of Global Health
Maria Small, MD, MPH
Associate Professor of Obstetrics and Gynecology, Obstetrics and Gynecology, Maternal Fetal Medicine
Haley Moss, MD, MBA
Assistant Professor of Obstetrics and Gynecology, Obstetrics and Gynecology, Gynecologic Oncology
Member of the Duke Cancer Institute, Duke Cancer Institute
Sarahn Wheeler, MD, MHSc
Associate Professor of Obstetrics and Gynecology, Obstetrics and Gynecology, Maternal Fetal Medicine
Vice Chair of Diversity, Equity and Inclusion for Department of Obstetrics and Gynecology
In addition, mentors in the department, like Dr. Cannon, are committed to career development in this context and have helped connect health equity curriculum trainees with experts in health equity across the nation.
Additional Opportunities to Expand Understanding
Beyond the health equity curriculum, trainees have the opportunity to engage in other health equity efforts led by our faculty, such as Project CHECKERS, a community-engaged participatory research effort aimed at creating more equitable processes for oropharyngeal cancer detection and prevention in marginalized local communities.
Curriculum participants can also take part in Duke REACH Equity’s health disparities research curriculum, where participants are familiarized with health disparities research methodology.
“I hope to learn more about community engagement methodology from Dr. Cannon, Dr. Osazuwa-Peters, Leda Scearce, and the CHECKERS team. I believe that this is a powerful way to empower and build capacity for low-resource communities to engage in preventative care as it relates to head and neck cancer,” Dr. Frisco said.
“Through these experiences, I hope to not only aid in the identification of these disparities but also start driving efforts to reduce inequity through implementation science.”
Building on Success
The health equity curriculum has led to increased recruitment of both trainees and staff who are interested in these topics. We’ve seen more interest among every resident cohort since the curriculum began.
“As the faculty advisor, I could not be prouder of the health equity curriculum that the residents put together, Dr. Cannon said. “In addition, the support from departmental leadership, faculty, and residents has led me to believe that everyone understands its impact.”
The department is looking to build on the momentum of the curriculum.
“I think the next big step for the curriculum is to translate this knowledge into practical change for our patients,” Dr. Patterson said. “That's what we're currently working on: figuring out ways to advance people's ability to implement actual changes to improve care.”