The uneven distribution of health resources is not a new story. But in the field of otolaryngology, where the ability to hear, speak, breathe, and swallow defines one’s engagement with the world, the consequences are profound. For millions globally, limited access to otolaryngologic care means more than just untreated disease—it means exclusion from education, employment, and social connection. A child with undiagnosed hearing loss struggles in school, not because they lack ability, but because they were never provided the hearing aids that could unlock their potential. A patient with an untreated airway disorder fights for every breath in a system that offers no specialists or equipment necessary to intervene. These are not rare tragedies but everyday realities in places where otolaryngology care remains an afterthought.
Dr. Rolvix H. Patterson, a PGY-5 research resident at Duke's Department of Head and Neck Surgery & Communication Sciences, has worked to document gaps in otolaryngologic care. As a 2023-24 NIH Fogarty Global Health fellow and Vice President of the Global OHNS Initiative, he has co-led large research teams to publish three recent manuscripts that emphasize the urgent need to invest in local training, to equip operating rooms in resource-constrained settings, and to address barriers that keep millions from the care they need.
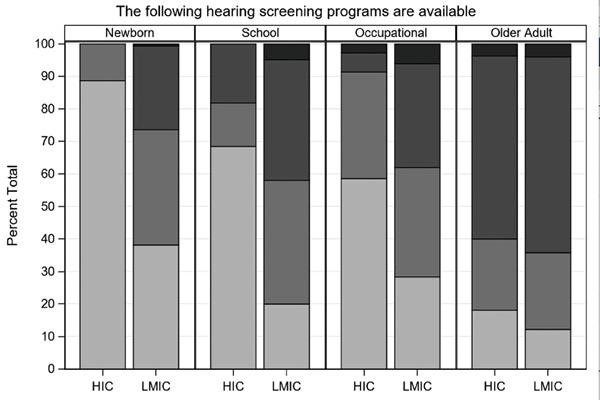
The first paper, titled “Access to Ear and Hearing Care Globally: A Survey of Stakeholder Perceptions from the Lancet Commission on Global Hearing Loss,” was published in the Otology & Neurotology journal. This study aimed to understand global access to ear and hearing care (EHC) to guide future policies. Researchers conducted a survey, gathering responses from 125 stakeholders in 59 countries, including healthcare professionals and individuals affected by hearing loss. The survey revealed that high-income countries (HICs) generally have better access to EHC resources compared to low- and middle-income countries (LMICs). HICs reported having more EHC professionals, training programs, and support services. The study concluded that systemic barriers limit EHC access, especially in LMICs, highlighting the need for urgent policy changes to improve global EHC access.
The second paper, “Otolaryngology–Head and Neck Surgery Training and Service Delivery: An International Survey,” was published in Laryngoscope Investigative Otolaryngology. This study highlights global disparities in otolaryngology training and service delivery, emphasizing the need for equitable access to training resources. The objective was to describe how the quality, content, and location of otolaryngology training impact care delivery worldwide. An online survey was conducted among otolaryngologists, distributed via professional societies and social media. Participants included otolaryngologists from all seven World Health Organization regions. The survey found that HICs have better access to subspecialty training and educational resources, as well as greater confidence in performing several complex procedures. Addressing these disparities is crucial for improving global otolaryngology care.
The third paper, “Essential Equipment for Baseline Otolaryngology-Head and Neck Surgery Care: A Global Cross-Sectional Survey,” was also published in Laryngoscope Investigative Otolaryngology. This study aimed to assess the availability of essential surgical equipment for OHNS across different income groups. A survey of 146 otolaryngologists revealed significant disparities between HICs and LMICs. LMICs, especially in Africa and South-East Asia, had less access to crucial equipment. The results showed significant differences in the availability of otologic, rhinologic, and endoscopic airway equipment between HICs and LMICs. Commonly used equipment like tympanomastoidectomy tools and rigid bronchoscopes, as well as specialized equipment like functional endoscopic sinus surgery tools and cochlear implants, were less available in LMICs. These findings highlight the need for targeted investments to improve surgical infrastructure in low-resource settings.
This research highlights the critical gaps in global otolaryngology and EHC, emphasizing the need for policy changes and strategic investments. Strengthening training programs, improving access to vital surgical tools, and incorporating hearing care into healthcare systems are evidence-based measures are key to reduce the burden of untreated diseases and ensure that more individuals receive the care they need.