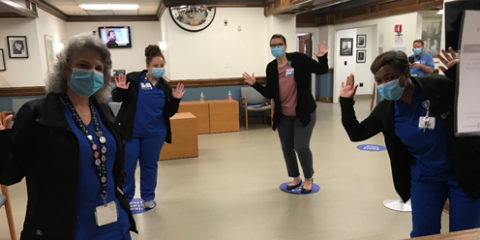
Photo from left to right: Kitty Lockner, RN, Cami Cunningham, Nurse Manager, Janelle Blossingham, Nurse Manager, and Ramona Basnight, COD.
This story is part of an ongoing series of reflections from Duke Surgery faculty and staff.
Nurses are generally in close contact with patients during their care and always have to remain alert in case an emergency arises. For nurse manager Cami Cunningham, BSN, RN, the COVID-19 pandemic showed just how vigilant and cooperative she and her team were during an unprecedented time.
As the nurse manager for the Department of Head and Neck Surgery & Communication Sciences (HNS&CS), Ms. Cunningham oversees the daily operations of its clinics. She ensures that the workflow, staff, and providers are in good shape to function for the day, troubleshooting at all times. This is especially true once the pandemic hit and protocols started to change.
“Mid to late March was when everything came down the line as far as change, especially with protocols because of COVID-19,” says Ms. Cunningham. “Basic protocol, such as limiting visitors and patients within the clinics, hit us fairly fast. One day we were working at a normal pace and the next it’s completely different.”
At the beginning of the pandemic, the restriction of patients visiting the clinics resulted in a significant decrease in volume when they would see less than 10 patients, whereas they would see about 70-80 patients a day on average. The only patients who needed to visit the HNS&CS clinics were cancer patients, whereas the majority of patients used the telehealth option.
“This was a collaborative effort with the nursing staff, providers, staff assistants, and front desk staff to ensure that patients were rescheduled or switched to telehealth visits,” says Ms. Cunningham. “These telehealth visits were a huge positive change that benefited our workflow as well as the convenience of our patients who do not need to visit the clinics.”
The number of patients and visitors in the clinic waiting rooms was also affected with these new protocols. Now, only one visitor is allowed per patient and a new method is used in the waiting rooms to follow social distancing guidelines.
“We had to implement these little dots in our waiting room to make sure patients are socially distanced when they’re in line,” says Ms. Cunningham. “Even when they’re sitting down, dots are placed to help them practice social distance and to further help, we reduced the number of chairs in the waiting room from 30 odd chairs to 10 chairs.”
With all these drastic changes that Ms. Cunningham and her team had to go through, communication between the nursing staff, faculty, residents, front desk, and patients was vital to ensure everyone’s safety. Part of their communication tactics is holding weekly calls as a team to discuss any changes from nursing providers, resident changes, and any updates on protocols from leadership.
“Communication between every small team has been tremendous and helpful,” says Ms. Cunningham. “It takes a collaborative effort and with one missing piece, it’s going to be much more difficult for us to do our job. Thankfully, there have been no major issues.”
Now that a few months have passed since the start of the pandemic, many of the protocol changes implemented have remained and become an everyday practice even when a sense of normalcy started to return within the HNS&CS clinics.
“Change is good and sometimes change isn’t necessarily great either, especially during this time, but you know that’s what we’re supposed to do” says Ms. Cunningham. “We’re supposed to adapt to whatever situation we’re put in and I think our group did a really great job at it.”