As members of a new department, faculty and staff in the Department of Head and Neck Surgery & Communication Sciences eagerly anticipated rapid progress and development throughout 2020 in becoming a model department.
When the coronavirus pandemic hit in early 2020, plans needed to be altered. The safety of the department’s faculty, trainees, staff, and patients became priority. Most of the staff started working from home. Clinical cases were put on hold or rescheduled. Safety guidelines for faculty, staff, and trainees working at the hospital constantly changed.
In a year filled with stress and anxiety, giving the best medical care and attention to patients remained a top priority, along with continuing to connect with the community. It didn't keep the faculty, staff, and trainees of HNS&CS from their journey to become an exemplary department.
Below is a timeline that recaps not only key global news concerning the COVID-19 pandemic, but the experiences that various members in HNS&CS encountered throughout 2020.

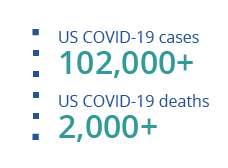
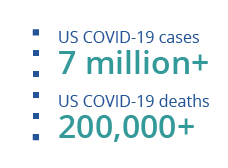
In January 2020, the United States announced its first confirmed coronavirus case. By the end of the month, the World Health Organization (WHO) declared the outbreak that started in Wuhan, China, a global public health emergency.

Howard W. Francis, MD, MBA
Chair, Department of Head and Neck Surgery & Communication Sciences
"In January 2020, when the first cases of COVID-19 were reported in the United States, synergy within our newly formed Department of Head and Neck Surgery & Communication Sciences was hard at work. In our first six months as a department, we had accomplished much: laying the groundwork for an expanded network of patient care through community clinics, increasing our research portfolio with funding from the National Institutes of Health and the Patient-Centered Outcomes Research Institute, adding a two-year research track to the otolaryngology residency program, creating a solid administrative infrastructure for department support, focusing on our reputation through the launch of a new website, and much, much more.
These focused, diligent, and collaborative efforts in the second half of 2019 did more than lay the foundation for a thriving department—they created a stronghold for us to weather the looming storms that were forming on the horizon."

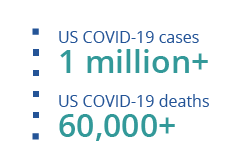
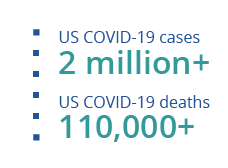
At the beginning of February, WHO announced that the disease caused by the coronavirus, SARS-CoV-2, would be officially known as COVID-19.
Toward the end of the month, the first recorded coronavirus death in the United States was confirmed.

Joshua Smith, MMS, PA-C, DFAAPA
Assistant Clinic Director, Division of Communication Sciences
"When the COVID-19 pandemic hit in early 2020, we had to change the way we ran our clinic. We worked with our Duke Infectious Disease team to frequently update our clinic procedures to match the emerging recommendations from the Centers for Disease Control and Prevention (CDC) and this changed rather frequently. Our leadership team met on a regular basis to make sure that we had the proper personal protective equipment (PPE) and that we were able to bring patients into clinic safely. While this was at first a hectic, confusing, and scary time, with experience we were able to transform our clinic experience into one that was safe and efficient."

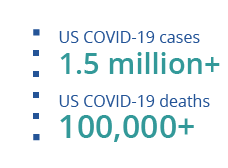
On March 11, WHO declared that the coronavirus outbreak was now a pandemic. Toward the end of the month, North Carolina Governor Roy Cooper announced plans for a stay-at-home order for the state.
Medically, the U.S. Food and Drug Administration had authorized the emergency use of a rapid coronavirus test that could give patients their results in 15 minutes.

Irish Hamilton
Department Chair's Administrative Assistant
"In March, our biggest transition was moving to working remotely. What was particularly challenging was making sure that everyone had the right technology to continue to work efficiently and effectively. There was quite a bit of rescheduling and moving our patients in the beginning and the bulk of that responsibility fell on the assistants. Working remotely has actually been busier than working in the office. We've had to come up with creative ways and learn new skills to be productive. That learning hasn't stopped as we continue to work remotely. No one really asks how we get things done, they just expect us to get it done. Our group has done a very good job of adapting, learning, and progressing with the remote work concept."

David Kaylie, MD
Vice Chair of Clinical Operations
"In March of 2020, we had to abruptly put a halt to all but the most urgent surgeries at Duke. This required a massive effort by a wide range of people. Our immediate intention was to protect the safety of patients and our staff. It is a testament to the quality of our Duke family that we were able to come together to get this job done."

Seth Cohen, MD, MPH
Associate Vice Chair of Clinical Operations
"We spent many weekends and evenings in March 2020 determining the initial steps, which were modified over time as the scientific community at large and the Duke COVID-19 expertise grew over time. Trying to determine protocols for infection prevention and patient and staff safety during the pandemic was certainly a challenge. This was a huge team effort involving my colleagues representing all our divisions, the infection prevention nurses, and infectious disease colleagues. Understandably, there was a lot of anxiety around the unknown of COVID-19 and its associated risks. With a great group of individuals, we evaluated the evolving literature, assessed our local COVID-19 epidemiology, had expert opinion discussions, inquired about practice patterns at other institutions, and aligned our recommendations with Duke Infection Disease and Infection Prevention."

Bradley Goldstein, MD, PhD
Vice Chair of Research
"Our labs were completely shut down with little notice, bringing most basic science work to a halt for many weeks."

David Straka, MD
Otolaryngology Resident
"Things changed quite a bit initially in March with small groups of residents rotating each week to minimize the chance of infection spreading. We were separated in a way we had never been."

Dehra McGuire, MD
Otolaryngology Resident
"March 2020 is the infamous month that felt like 3 years. It was a strange time to be the ENT consult resident. As otolaryngologists, pretty much our entire practice revolves around the respiratory tract, which happened to contain the highest viral loads for COVID-19. While we received fewer consults as people began to avoid going to the hospital, each consult carried a new sense of risk. We were still without a reliable COVID-19 test at this point and PPE guidelines were changing rapidly. This was the month before we split into platoons that rotated working in and out of the hospital.
Like many other otolaryngology programs around the country, we began to defer elective inpatient consults like vocal cord evaluations for hoarseness and how we managed other non-urgent airway consults to protect our resident cohort. Our faculty went to great lengths to keep us informed and safe. There were a lot of discussions about cancelling OR cases, which did end up significantly affecting my next rotation. This was certainly a month of uncertainty and not without fear, especially with reports rolling in of PPE shortages and international ENT doctors getting very sick around the world."

Cami Cunningham, BSM, RN
Nurse Manager
"Initially in March when the pandemic really hit and affected healthcare, much of my day was spent downsizing clinic volume to less than 15 patients/day, triaging emergent patients to be seen in clinic, redeploying staff to COVID-19 work areas in need, and staying in the know of minute by minute changes in regards to policies and protocols that included PPE and infection prevention changes. These included universal masking that was required for all staff and patients. I also collaborated with providers in regards to ENT specific changes. All of this required communicating the changes to staff as we got updates, which caused a lot of stress amongst the team to keep up with current practices."

The White House and the Centers for Disease Control and Prevention (CDC) recommended that Americans wear cloth face masks in public to prevent further spread of the COVID-19.
The CDC also expanded the list of recognized COVID-19 symptoms to include chills, repeated shaking with chills, muscle pain, headache, sore throat, and the loss of taste and/or smell.

Eileen Raynor, MD
Chief, Division of Pediatric Otolaryngology
"During April, we all really felt the impact of COVID-19 as all elective surgery and clinic visits were suspended. Our team had done some telehealth video visits prior to the pandemic but we rapidly accelerated our ability to use telehealth so patients would avoid significant gaps or delays in care.
Duke had several new platforms via EPIC for telehealth and I spent much of April training our speech pathologists, audiologists, and surgical trainees on how to use the system. There were frequent conference calls, updates to the flow and changes to how telehealth was accessed. We created PowerPoint presentations to help with troubleshooting problems around the virtual care platform. Although we had no in-person visits other than inpatients who still needed care, we remained extremely busy ramping up the telehealth option."

Gina Vess, CCC-SLP, MA
Director of Clinical Operations & Staff Development, Duke Voice Care Center
"In April, our speech pathology group was largely working from home, tirelessly gathering information from Duke, our department, our national organization, and our Speech Language Pathologist colleagues in COVID-19 hotspots. Information on the virus appeared to change on a daily basis. What appeared to be high priority one moment, was ever changing as the pandemic evolved. As a leader, I’ve never felt so much weight as I did in that moment, being concerned about our patients' and staff’s safety, and that all of the procedures we do in the nose, throat, and trachea, where the COVID-19 was in the highest concentrations. It was also unclear if Duke would have to lay off staff. We’ve learned so much now and have robust safety protocols in place, but at that point in time, we could not foresee how this situation would turn out. It brings tears just looking back at my emails from last April."

La Wanna Bochert, MBA
Health Center Administrator
"At the onset of COVID-19, there was a lot that we did not know. Implementing CDC recommendations that help keep staff, providers, and patients safe is my number-one priority. In April, we continued to revise best practices weekly. Maintaining open lines of communication was the key to ensuring that everyone was well informed and safe. We used our daily huddle to provide updates, answer questions, and talk through process changes. We were only seeing urgent patients in the clinic. Duke implemented visitor restrictions, and we rolled out a screening process for patients and staff."

Michelle Hartzog, AuD
Clinical Audiologist
"I returned from maternity leave early in the pandemic and the structure of scheduling and appointments had completely changed in the months during my leave. We had a reduced schedule and were given the difficult task of deciding which patients were 'essential.' There was a constant sense of underlying unease during conversation and testing with patients, especially while we were in the confined space of the sound booth, where there is little circulation of air and distance cannot be maintained."

Dawn Raggio
Service Access Manager, Duke Otolaryngology of Raleigh
"Just prior to COVID-19, I took the Service Access Manager position in the clinic, which left a vacancy in the Financial Care Counselor position. We also had two staff members take positions at other locations. This put us at half-staff at the front desk. Our two patient service associates that remained were rotating one week in clinic, one week off. We utilized nursing staff to assist us in rescheduling all patients three months out. Our clinic was open half days in the mornings and only for emergent patients. Duke also implemented a hiring freeze. We could not have done it without the front desk and nursing team working together!"

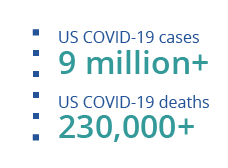
On May 1, the U.S. Food and Drug Administration (FDA) granted the emergency use authorization for the drug remdesivir to treat people with severe COVID-19.
Walter Lee, MD, MHS
Chief of Staff
"We have been holding frequent forums with the department on zoom because getting timely communication and information out to everyone was important. We also tapped the collective experience and ingenuity we have in HNS&CS to help troubleshoot and solve problems. During these forums, we took a moment to share something someone was grateful about, something to think about, and something to smile about, which helped to keep us all grounded and keep the big picture in view."

Trinitia Cannon, MD
Vice Chief, Division of Head and Neck Surgical Oncology
"It has been very exciting, but difficult to launch a new HNS&CS cancer program in the middle of COVID-19. In the pre-COVID-19 era, I would have gone out and knocked on the office doors of all of the local and regional providers that I had hoped to establish a referral relationship with. When the pandemic hit, all face-to-face connections were shut off. I had to find new ways to introduce myself to my new community. With the help of the marketing team at Duke, I launched a Doximity campaign to introduce myself. In addition, I am also launching some community talks on topics of interest such as advanced skin and oral cavity cancers. This is helping me spread word about my practice and I am getting referrals and establishing important relationships in Raleigh and Wake County."

The World Health Organization (WHO) clarified that asymptomatic people with COVID-19 could still easily spread the virus without knowing.

David Straka, MD
Otolaryngology Resident
"Over time as we adapted, our clinical volumes gradually increased to pre-COVID-19 levels and all of us residents were together again. I feel very fortunate to be able to continue working the way we do. Unlike others who are stuck working from home in less than ideal circumstances, I get to come to the hospital every day and perform the job I love with the people I love. I would also add that although residency by itself can make seeing family challenging, COVID-19 has added to the barriers. I have not been able to see my family during this time like before but, thankfully, as residents we have each other to rely on as family now more than ever."

Angela Canady-Blaylock, RN
Nurse Manager, Duke Otolaryngology of Raleigh
"It was such an uncertain time. The weekly department forums on Zoom were super helpful to me. It was always nice to have those meetings to voice concerns and learn tidbits about how we were going to function day to day. Our HCA was on maternity at the time and I was the clinic leader. It brought comfort to me knowing there were other leaders to go to, knowing you're not out there on your own. Hearing the game plan each week made me feel confident. It meant everything."

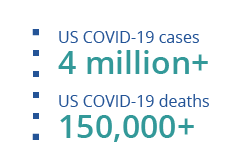
On July 7, WHO acknowledged the scientific evidence of the airborne spread of COVID-19.

Dawn Raggio
Service Access Manager, Duke Otolaryngology of Raleigh
"In July, we were back to operating at full clinic. We had changed the lobby to reflect social distancing and had started using a WIFI phone to implement patients checking in from their car. We again utilized front desk and nursing staff to call or send MyChart messages to all patients informing them of the new check-in process. We hired two temps to assist at the front desk as we were still in a hiring freeze. We interviewed a Financial Care Counselor from another clinic and began working with HR to hire as an exception during the hiring freeze."

David Kaylie, MD
Vice Chair of Clinical Operations
"When it was deemed safe, we were able to reopen the operating rooms, and by July we were able to get to the point where there were no restrictions on what surgeries could be done. There are still patients who are waiting until vaccinations are more widespread before they choose to come back for their elective surgeries, but a large majority of patients have found Duke to have superior attention to safety and have resumed their care at Duke. We continue to strive for the safest top-quality care for our patients."

Operation Warp Speed, initiated by the U.S. government to accelerate the development and distribution of the COVID-19 vaccines, announced that a COVID-19 vaccine would likely be available by spring 2021.

Gina Vess, CCC-SLP, MA
Director of Clinical Operations & Staff Development, Duke Voice Care Center
"Our hard work in the early months of the pandemic had started to pay off by August. By mid-May, telehealth policy was in place, and the Duke Voice Care Center Speech Language Pathologists were happy to provide services for patients through videos in the comfort of their own homes. This allowed even greater access to care than expected, considering patients in rural counties and long distances could see our voice specialists remotely. As with many relationships, the pandemic also helped clarify our resolve. We were tested in a way no one expected, and I believe we are stronger for it."

Rachel Burch, PA-C
Physician Assistant, Duke Otolaryngology of Raleigh
"COVID-19 certainly threw a wrench into my start date, which was originally slated for May 2020. Due to desired decrease in patient contact for patient and staff safety we agreed the best thing to do would be to push back this date to July 2020, but it wasn't until August when I was able to interact with patients. When I thought about practicing as a new graduate, I never imagined I would be starting my first job in my medical career during a pandemic. I expected this would be difficult as I thrive off patient contact and seeing the corners of a patient’s mouth curl into a smile. I knew with the pandemic this simple thing would be hard to come by, not only with increased PPE but the general tension this pandemic has provoked from patient to practitioner. Simple things I took for granted like being able to familiarize myself with a coworkers' faces, most of which I have never seen fully in person. Initially, I was concerned perhaps my voice may not be heard regarding COVID-19 concerns, but Duke Otolaryngology of Raleigh has allayed these concerns and made sure all staff members were part of the conversation and concerns were heard."

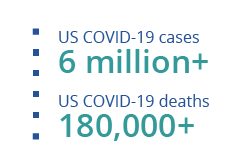
During this month, the CDC released a report stating that dining out increased the risk of contracting COVID-19.

La Wanna Bochert
Health Center Administrator
"By September, things were going well. We were back to our pre-COVID-19 clinic volume. Our screening process was revised and is now working well. The team pulled together to take care of our patients and each other. We streamlined safety protocols to keep everyone safe that remains in place today."

Cami Cunningham
Nurse Manager
"Fast forward to September, clinic volumes are back to normal with 70–90 patients per day. During the summer, staff returned to the clinic full time to serve the increasing patient volume. Communication about changes still continues; however, these changes typically occur only twice a week hospital-wide. Communication remains important with clinical staff, providers, and PRMO staff. The PPE changes have slowed down and have become more standardized, where certain ones are worn based on what is being done for the patient at the time of the appointment. Waiting room remains at 10 chairs to continue to promote social distancing. We still continue the universal mask policy for all who enter the building."


Rachel Burch
Physician Assistant, Duke Otolaryngology of Raleigh
"Initially I questioned how I would be able to connect with a patient without being able to see their face and vice versa. This seemed impossible. However, over the months I began to rely on other things to cultivate connection such as voice inflection, and a whole lot of eyebrow with eye expressions! It is still tough sometimes, but we are all in this together and I feel the camaraderie with both patients and coworkers. Some roadblocks exist in working with those patients who have impaired hearing and rely heavily on their ability to lipread. Due to masking this has been a challenge; thankfully, clear masks were developed, and I can utilize these for improved communication with these patients. I feel over the months with changing CDC guidelines we adapted quickly in response to keep our staff and patients safe. Sometimes this unfortunately meant temporarily turning patients away due to their COVID-19 status or suspicion in protection of other patients and staff members. In the field of medicine, which is in constant state of evolution, coupled with guidelines and COVID-19 numbers ever changing I find that my words of the 2020 year are diligence, flexibility, and grace."

Irish Hamilton
Department Chair's Administrative Assistant
"Adaptation has been continuous. Keep in mind our "workstations" are all different now. Not everyone started out with the same equipment such as laptops, computers, or printers. There were and still are tasks that needed to be done, but had to figure out how to get these things done with fewer resources at home. Since October, we've been provided laptops and for some that in itself has been an adaptation. They weren't accustomed to using laptops and its usage at home is different than being on a docking station at home. We've had to adapt with the handling of medical records which in itself can be a major task. There's a lot that goes on behind the scenes before our faculty members see a patient in clinic. Making sure those tasks are still accomplished from working remotely hasn't been easy, but we are continuously trying to improve the process."

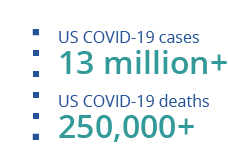
In November, the FDA authorized the first at-home COVID-19 test that would give users results quickly.
For the people in the United States, the CDC warned Americans to refrain from traveling for the Thanksgiving holiday.

Michelle Hartzog, AuD
Clinical Audiologist
"By November, our appointments were at full or over capacity and patients had definitely become weary of the safety protocols. There was fatigue in mask wearing and an overall sense of depression at the approaching holidays and inability to spend time with family. Patients had to be reminded to keep on masks during testing and I often felt as a provider that patients didn't realize their mask wearing was for my safety as well. Many patients expressed ongoing difficulty with the retention of their hearing aids with the mask straps. Others had lost or stopped wearing their hearing aids at all, as their social encounters were limited and they were unable to handle the mask and hearing aids behind their ears."

Bradley Goldstein, MD, PhD
Vice Chair of Research
“When it was safe for us to go back to our labs a few months ago, some of us focused our research to understand COVID-19. Since I work on olfaction, the importance of COVID19-induced smell loss was an obvious focus that brought more interest to our field. We continue to work towards understanding and treating this problem.”
Early in December, the United Kingdom (UK) identified a new variant of the coronavirus, which appeared to be more transmissible. Similarly, a second new variant was identified in South Africa, but it has shown to affect young people more than the UK variant.
The biggest development was the authorization for the emergency use of Pfizer’s and Moderna’s COVID-19 vaccines. These vaccines were distributed a few days later once the FDA gave its approval.

Dr. Eileen Raynor
Chief, Division of Pediatric Otolaryngology
"By December, most clinic in-person volumes had returned to almost pre-COVID-19 numbers. We continued to offer telehealth video visits, especially for patients who are at high risk for COVID-19 or have to travel a distance. The patients seem to be grateful that this has remained an option for them, especially as we continue to have an increase in cases in NC as well as continued visitor restrictions that prohibit families from bringing their other children to the office visits.
If I had to put it succinctly, I would say telehealth is a viable option for many patients and does improve care overall; however, it does not eliminate disparities that exist within our system due to lack of reliable broadband access across the state. The pandemic has certainly highlighted the concern about health inequity."

With the emergence of the two new coronavirus variants, tests showed that the Pfizer vaccine would be effective against them.

Dr. Dehra McGuire
Otolaryngology Resident
"New year, same virus. Thankfully, we now have reliable POC tests that can screen our patients quickly and accurately. Each patient now gets a COVID-19 test before they undergo surgery, which leads to a significant portion of cancellations. Most patients we’ve consulted for have been tested as well, and we are back to seeing all consults as usual. We residents carry our 3D printed face shields that we can clean between patients rather than disposable shields. I’m so relieved to be vaccinated. I’m rotating at the VA now, and the veterans are starting to receive their vaccinations as well. Our surgical case volume is still low because nurses have been pulled from the OR to care for patients on the floor, resulting in fewer OR days. Many of our appointments are being converted to telephone visits as patients are still very hesitant to come to the hospital unless absolutely necessary, but I can feel things slowly, very slowly, returning to some semblance of normality. At this point, I’m not sure we’ll ever go without masks in ENT clinic again."

Howard Wayne Francis, MD, MBA
Chair, Department of Head and Neck Surgery & Communication Sciences
COVID-19 Global News Sources:
NBC News - "Coronavirus Timeline: Tracking the critical moments of COVID-19"
Give to Duke Head and Neck Surgery & Communication Sciences
A gift to the Department of HNS&CS is a gift of knowledge, discovery, and life.