Dr. Nosayaba (Nosa) Osazuwa-Peters, BDS, PhD, MPH, CHES, Associate Professor in the Department of Head and Neck Surgery & Communication Sciences at the Duke University School of Medicine and a member of the Duke Cancer Institute, is the senior author behind a newly published study in JAMA Network Open that reveals significant disparities in the use of antidepressants and anxiolytics among cancer survivors in the United States.
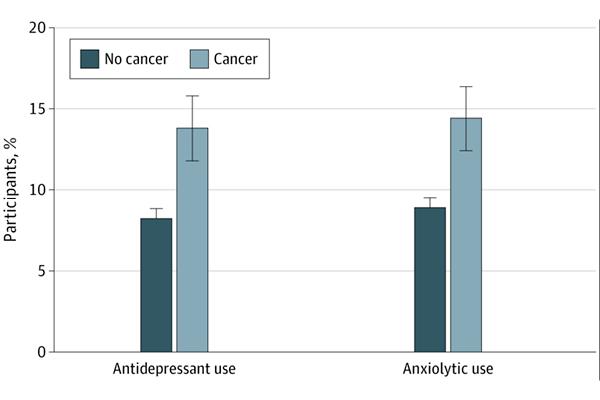
Using data from the National Health Interview Survey collected between 2016 and 2018, Dr. Osazuwa-Peters and colleagues found that cancer survivors are more likely to use medications for depression and anxiety than those without a cancer history. His research also highlights troubling racial and ethnic gaps in access to these treatments, underscoring the need for more accessible mental health care in oncology.
After adjusting for sociodemographic factors, the analysis showed that non-Hispanic Black cancer survivors had notably lower odds of using antidepressants and anxiolytics compared to their non-Hispanic White counterparts. The findings also highlighted differences in medication use based on cancer type, with survivors of brain and pancreatic cancers being the most likely to use these medications. Insurance status played a role as well, with individuals on Medicare or Medicaid more likely to report anxiolytic use than those with private insurance.
These results underscore the importance of integrating mental health care into cancer survivorship plans and addressing systemic inequities that affect access to treatment. As the number of cancer survivors in the U.S. continues to grow—now exceeding 18 million—ensuring equitable access to mental health support is more urgent than ever. Dr. Osazuwa-Peters has led NIH-funded work aimed at mitigating suicide and other poor mental health outcomes in cancer survivors. Cancer survivors, and especially head and neck cancer survivors, have higher rates of suicide compared to people in the general population. Depression is a known risk factor for suicide, which was the motivation for conducting the current study.
This study adds to a growing body of evidence that mental health must be a central component of cancer care, not only during treatment but throughout survivorship. The full article is available through JAMA Network Open.