Dysphagia, or difficulty swallowing, can lead to serious health problems. While its impact on general health is well-known, its effect on surgical outcomes has not been thoroughly studied.
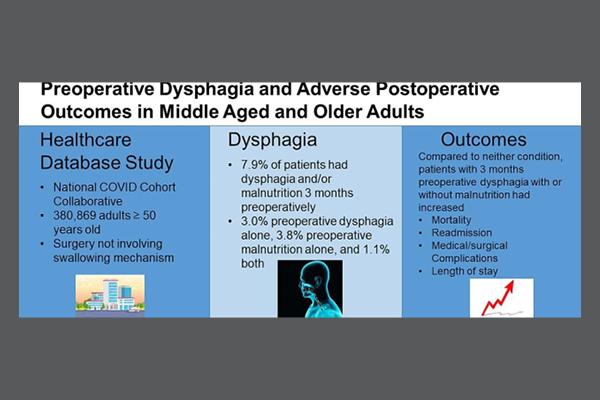
Harrison N. Jones, PhD, BRS-S, MA, Associate Professor and Seth Cohen, MD, MPH, Professor in the Duke Department of Head and Neck Surgery & Communication Sciences, conducted a retrospective, observational study using data from the National COVID Cohort Collaborative (N3C) database, which includes electronic health records from over 75 health systems in the United States.
The study focused on patients aged 50 and older who underwent surgeries not involving the swallowing mechanism. The main predictor was the presence of dysphagia with or without malnutrition in the three months before surgery. Statistical models were used to assess the association between these conditions and outcomes such as mortality, readmission, and medical/surgical complications. The study was published in the Journal of Clinical Anesthesia in November.
The study included 380,869 adults with an average age of 66 years. About 8% of these patients had dysphagia or malnutrition before their surgery. The findings revealed that patients with preoperative dysphagia with or without malnutrition had higher odds of dying within a year, being readmitted to the hospital within 90 days, and experiencing medical or surgical complications compared to those without these conditions.
The study concluded that patients with preoperative dysphagia had worse outcomes after surgery. These findings underscore the need for integrating dysphagia screening and intervention into routine preoperative protocols to mitigate the risk of adverse postoperative outcomes.
Jones and Cohen have previously highlighted disparities among patients with dysphagia and other findings from this paper provide additional support. For example, prevalence rates for preoperative dysphagia/malnutrition were higher in Black versus White and Asian patients, in males compared to females, and in Hispanic or Latino patients.
Moreover, another paper in preparation by Jones and Cohen in collaboration with their multidisciplinary research team focuses on disparities in the assessment and treatment of dysphagia/malnutrition in this population. These data show that women (compared to men), Asian patients (compared to White and Black patients), and Hispanic/Latino patients were less likely to receive assessment /treatment for dysphagia/malnutrition. They also examined the effects of assessment/treatment for dysphagia/malnutrition in the perioperative period on postoperative outcomes. Those who received assessment/treatment had lower odds for 30-day, 90-day, and 1-year mortality, but higher odds of readmission and complications.
These findings highlight the importance of addressing dysphagia and malnutrition in surgical patients to improve their postoperative outcomes. Early screening and intervention can play a crucial role in reducing the risks associated with these conditions.
To refer a patient, call Duke's Consultation and Referral Center at 800-633-3853 or log into Duke MedLink.