A recent study published in Vaccine, highlights the impact of the Affordable Care Act (ACA) on HPV vaccination rates in the United States. The study reveals significant improvements in vaccination uptake, particularly among racial and ethnic minorities, following the implementation of the ACA.
A team of researchers from various universities, including May Z. Gao from Duke School of Medicine and Nosayaba Osazuwa-Peters, BDS, MPH, PhD, from the TORCHE Lab at Duke Department of Head and Neck Surgery & Communication Sciences conducted the study.
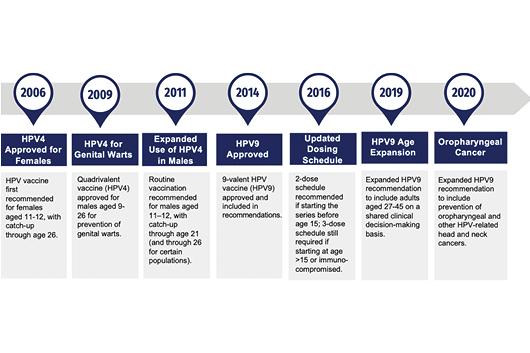
Human papillomavirus (HPV) vaccination is crucial for preventing certain types of cancers. Despite increased vaccination rates in the U.S., they still fall short of the Healthy People 2030 goal. The ACA aimed to improve access to preventive healthcare services, including HPV vaccination, by reducing the cost of care.
Researchers analyzed data from 29,216 adults aged 18-26 from the National Health Interview Survey between 2011 and 2017. They compared vaccination rates and factors such as regular doctor visits and health insurance status before (2011-2013) and after (2014-2017) the ACA was implemented. The analysis was adjusted for factors like poverty, education, marital status, other health conditions, sex, and location.
Key Findings:
- The number of individuals receiving at least one dose of the HPV vaccine increased by 43% after the ACA was implemented, rising from 3.9% to 5.5%.
- Significant increases were observed among non-Hispanic White (55% increase) and Black individuals (59% increase).
- The completion rate for at least two doses of the vaccine rose from 12.5% to 17.8%.
- Hispanic individuals saw a notable increase in vaccine completion from 7.6% to 14.7%.
- There was a significant decrease in the number of uninsured individuals.
- The odds of completing the vaccination series increased for those with private insurance and Medicaid.
- Regular doctor visits also increased from 53.1% to 57.1%.
The ACA has been associated with increased HPV vaccination rates, especially among racial and ethnic minorities. This improvement is likely due to more people having health insurance and better access to regular doctor visits.
This study underscores the positive impact of the ACA on public health and highlights the importance of accessible healthcare in improving vaccination rates and overall health outcomes.