The Complications of Hearing Loss and the Importance of Its Risk Assessment


Howard Wayne Francis, MD, MBA, Chair of HNS&CS
Each day when we use masks as a barrier to protect ourselves from COVID-19, we also create another blockade—one that covers our mouths, muffles our voices, and makes communication for people with hearing loss even more challenging.
For ENT healthcare providers, who rely on clear communication with their patients to provide the best possible care, this new barrier further impairs communication in a population that may already have a high rate of hearing difficulties. This realization prompted several Duke faculty members to review the impact of hearing loss and breakdowns in communication on patient outcomes, reviewing how these difficulties may have impacted care even before the pandemic. Their findings reveal that there is a strong link between age-related hearing loss and post-operative complications. Now, they want to figure out why.
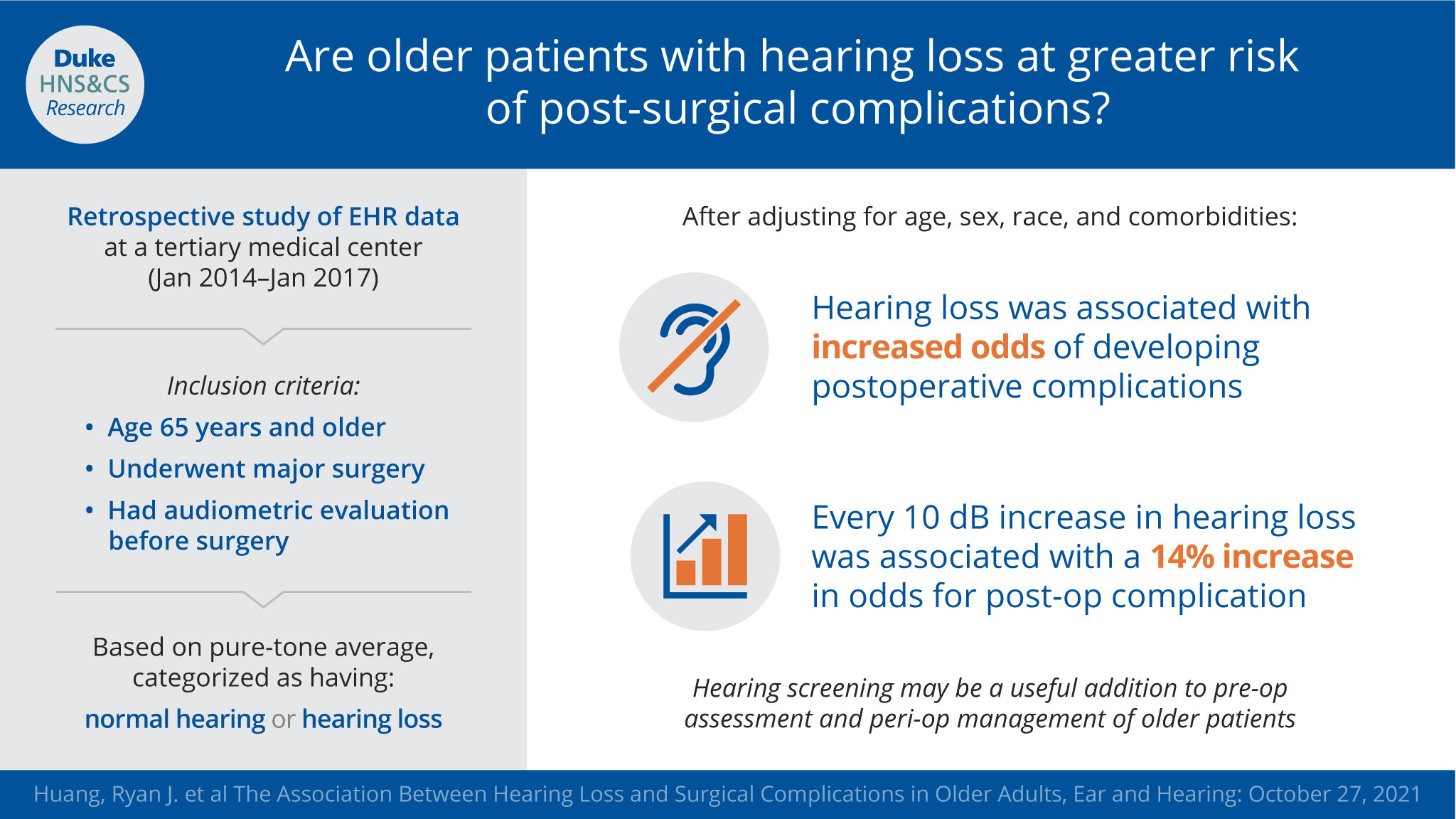
Ryan Huang, a 4th-year Duke medical student mentored by Howard Francis, MD, MBA, and Sherri Smith, PhD, AuD, published these findings in Ear and Hearing in 2021. Post-operative complications, hospital length-of-stay, and 30- and 90-day readmission rates were the areas of focus.
The study integrated two datasets—one from PYTHIA, a curated dataset of patient electronic medical record data from surgical patients at Duke University, and the other from Audbase, Duke’s specific audiological database—which led to an analysis revealing that complications increased by 14% for every 10 db increase in hearing loss.
Smith makes the research’s framework clear. “There’s something special about hearing loss that is alerting us to say, ‘This person may be at risk for some adverse outcomes, above and beyond all their other risk factors, that are often incorporated into risk assessment algorithms for surgical patients. But to our knowledge, hearing loss is not considered in some of the risk-based assessments.”
Should hearing screening be part of these assessments? This question must be asked in order to take all factors into account and deliver the best service possible to patients.
"To our knowledge, hearing loss is not considered in some of the risk-based [preoperative] assessments."
According to Drs. Francis and Smith, older patients undergoing surgery should be screened for hearing loss in order to proactively improve communication leading up to and throughout surgical care, and mitigation efforts including perioperative management that improve surgical outcome. Hearing loss impacts three specific areas: baseline overall health, vulnerability to the unavoidable biological stress of surgical care, and need for augmented communication.
Measuring hearing loss in patients can signal the necessity to shape care plans to minimize specific risks, “including managing chronic comorbidities, reducing polypharmacy, optimizing mobility and nutrition, and reducing delirium risk” (9). This personalization process follows what Dr Francis calls, a “growing emphasis in our healthcare system on maximizing quality and reducing cost, so called value-based care.”
Groundwork for Future Research
From their retrospective study, Drs. Francis and Smith are addressing hearing loss in the areas of patient-provider communication and risk-assessment. They currently are in discussions with health system leaders to explore ways to improve patient-provider communication in older adults and surgical outcomes.
Hopefully, this immediate and dynamic groundwork will lead to greater understanding of the medical implications of hearing loss and the demonstration of strategies that can improve outcomes and the patient experience. Designing care with the impact of hearing loss in the forefront is important and, as Drs. Smith and Francis have shown, increasingly necessary to ensure communication is accessible to all patients.